Cancer Immunotherapy
The immune system is a defense system that protects our body from harmful substances and microorganisms. Disorders of the immune system can occur due to factors such as stress, depression, bad habits such as alcohol/smoking, eating disorders, processed foods, environmental pollution, heavy metals, genetic predisposition, inactivity, and chronic health problems. Disorders in the immune system can increase the risk of cancer.
In recent years, treatments that strengthen the immune system have developed due to awareness of the importance of the immune system in cancer.
Medical and complementary treatments for the immune system can show more benefits when used in combination with each other. Unfortunately, in the fight against cancer a single weapon is often not enough, and medical treatments with the things the person will do can increase success.
In our clinic, effective anticancer immunotherapy drugs, vaccines, and complementary treatments for the immune system that we follow and treat include:
- Immunotherapy drugs
Immunotherapy drugs, such as: pembrolizumab, nivolumab, ipilimumab, atezolizumab, and avelumab, have been approved for use in the treatment of various cancers, including small-cell lung cancer, head and neck cancer, kidney cancer, melanoma, and bladder cancer in Europe and the United States.
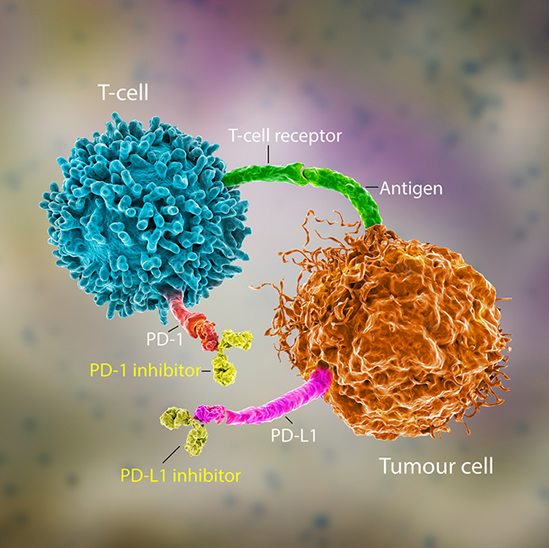
These drugs work by blocking the negative effects of CTLA4, PD-1 protein, and PD-L1 ligand on immune system cells, which normally suppress the immune system in cancer and prevent immune cells from destroying cancer cells. Immunotherapy drugs have been shown to provide clinical benefits as salvage therapy for cancer cases that are resistant to standard treatments and are generally more effective than chemotherapy with fewer side effects.
Reference:
1. Immune checkpoint proteins: a new therapeutic paradigm for cancer--preclinical background: CTLA-4 and PD-1 blockade. Semin Oncol. 2010 Oct;37(5):430-9.
2. Bansal P, Osman D, Gan GN, Simon GR, Boumber Y. Recent Advances in Immunotherapy in Metastatic NSCLC. Front Oncol. 2016;6:239.
3. Heinhuis KM, Ros W, Kok M, Steeghs N, Beijnen JH, Schellens JHM. Enhancing anti-tumor response by combining immune checkpoint inhibitors with chemotherapy in solid tumors. Ann Oncol. 2019 Jan 4. doi: 10.1093/annonc/mdy551.
2. Dendritic cell vaccines
Dendritic cell vaccines (DCV), also known as dendritic cell therapy, are new and powerful forms of immunotherapy in cancer treatment. An example of this treatment method is the Sipuleucel-T vaccine, which has been approved by the FDA for use in the treatment of prostate cancer in the United States.
Dendritic cells recognize and process foreign structures in the body and present them to T cells, the executor cells of the immune system, to initiate a strong immune response and begin the process of eliminating foreign structures. To prepare DCV, monocyte cells are first collected from the patient's blood, then transformed into dendritic cells in a laboratory setting. They are then cultured and returned to the patient to accelerate a stronger reaction from the immune system.
During the preparation of DCV, cancer-specific structures are often extracted from paraffin blocks taken from the cancer tumors and introduced to dendritic cells to help develop a cancer-specific response.
In mesothelioma, cancer that does not respond well to treatment, long-term disease control has been reported with the use of autologous tumor cell lysate-treated dendritic cancer vaccines in combination with metronomic cyclophosphamide treatment after conventional treatment.
In small cell lung cancer, a type of cancer with a high risk of recurrence after surgery, chemotherapy is a treatment that reduces the risk of recurrence in these patients. In a study, 103 patients with non-small cell lung cancer who had undergone surgery were divided into two groups; one group received standard treatment with chemotherapy, and the other group received chemotherapy and a dendritic cancer vaccine. Over 5 years, 48% of the patients in the group receiving only chemotherapy survived, while 81% of the patients receiving chemotherapy and a dendritic cancer vaccine survived.
In glioblastoma, an aggressive brain cancer, it has been shown that the use of a dendritic cancer vaccine prepared from tumor tissue in combination with conventional treatment extends the life span. DCV helps in the treatment of various cancers with minimal side effects and safe use.
Reference:
1. Koido S. Int J Mol Sci. 2016;17:6.
2. Abraham RS, Cytotherapy. 2016;18(11):1446-1455.
3. Cornellissen R, Am J Respir Crit Care Med. 2016;193(9):1023-31.
4. Kimura H, Cancer Immunol Immunother. 2015;64(1):51-9.
5. Jie X, Cell Biochem Biophys. 2012;62(1):91-9.
3. Lung-cancer vaccines
GM3(Neu5Gc) ganglioside is a cancer antigen structure found in cancer cells but not in healthy cells. The Racotumumab (Vaxira) cancer vaccine developed in Cuba may be effective against cancers that carry this protein.
The main goal of the Racotumumab cancer vaccine is to increase the immune system's response to GM3(Neu5Gc) ganglioside protein on the surface of cancer cells, allowing them to bind to it and subsequently identify and destroy the cancer cell. Because GM3(Neu5Gc) ganglioside protein is not present in normal healthy cells, the vaccine only affects cancer cells and does not affect normal cells.
Cancers that contain the GM3(Neu5Gc) ganglioside protein targeted by Racotumumab include (1-9):
Small cell lung cancer
Breast cancer
Esophageal cancer
Stomach cancer
Colon cancer
Rectal cancer
Pancreatic cancer
Liver cancer
Kidney cancer
Bladder cancer
Testicular cancer
Uterine cancer
Prostate cancer
Thyroid cancer
Sarcomas
Wilms tumor
Ewing sarcoma
Neuroblastoma
The anti-EGF vaccine is a cancer vaccine developed in Cuba.
Racotumumab and anti-EGF cancer vaccines have been approved for use in various countries for cancer treatment. The Racotumumab and anti-EGF cancer vaccines are approved for use in the treatment of advanced-stage non-small cell lung cancer that has responded to chemotherapy or radiotherapy (10). In suitable patients, we can prescribe and use the Racotumumab vaccine.
Clinical studies and case presentations indicate that the Racotumumab vaccine may be effective in other types of cancer and it is expected to be approved for use in these cancers in the future.
One of the main advantages of Cuban cancer vaccines is that they can extend the lives of cancer patients without significant side effects and provide long-term, high-quality life for some patients.
Reference:
1. Marquina G , Waki H , Fernandez LE , et al. Gangliosides expressed in human breast cancer. Cancer Res 1996;56:516551–71 .
2. Oliva JP , Valdes Z , Casaco A , et al. Clinical evidences of GM3 (NeuGc) ganglio- side expression in human breast cancer using the 14F7 monoclonal antibody labelled with (99m)Tc. Breast Cancer Res Treat 2006;96:115–21 .
3. Carr A , Mullet A , Mazorra Z , et al. A mouse IgG1 monoclonal antibody spe- cific for N-glycolyl GM3 ganglioside recognized breast and melanoma tumors. Hybridoma 2000;19: 241–7.
4. Zhong Y , Wu Y , Li C , et al. N-Glycolyl GM3 ganglioside immunoexpression in oral mucosal melanomas of Chinese. Oral Dis 2012;18:741–7 . [16] Blanco R , Rengifo E , Cedeno M , et al. Immunoreactivity of the 14F7 Mab raised against N-Glycolyl GM3 ganglioside in epithelial malignant tumors from digestive system. ISRN Gastroenterol 2011;2011:645641.
5. Blanco R , Quintana Y , Blanco D , et al. Tissue reactivity of the 14F7 Mab raised against N-Glycolyl GM3 ganglioside in tumors of neuroectodermal, mesoder- mal, and epithelial origin. J Biomark 2013;2013:602417.
6. Scursoni AM , Galluzzo L , Camarero S , et al. Detection of N-glycolyl GM3 ganglioside in neuroectodermal tumors by immunohistochemistry: an at- tractive vaccine target for aggressive pediatric cancer. Clin Dev Immunol 2011;2011:245181.
7. Blanco R , Dominguez E , Morales O , et al. Prognostic significance of N-Glycolyl GM3 ganglioside expression in non-small cell lung carcinoma patients: new evidences. Patholog Res Int 2015;2015:132326.
8. Hayashi N , Chiba H , Kuronuma K , et al. Detection of N-glycolyated ganglio- sides in non-small-cell lung cancer using GMR8 monoclonal antibody. Cancer Sci 2013;104:43–7.
9. Labrada M, Dorvignit D, Hevia G, et al. GM3(Neu5Gc) ganglioside: an evolution fixed neoantigen for cancer immunotherapy. Semin Oncol. 2018 Jan;45(1-2):41-51.
10. Hernández AM, Vázquez AM. Racotumomab-alum vaccine for the treatment of non-small-cell lung cancer. Expert Rev Vaccines. 2015 Jan;14(1):9-20.
4. Local Hyperthermia
One of the main reasons for the failure of cancer treatments is the ability of cancer cells to repair the damage caused by medical treatment. Cancer cells can repair damage caused by medical treatments by activating various repair mechanisms. This repair ability can be inhibited by hyperthermia or heat therapy.
Hyperthermia involves the application of heat to the tumor region at temperatures between 42-44°C, which helps to prevent repair. Additionally, applying 42-44°C heat to cancer masses using 13.6 MHz radiofrequency waves can lead to the secretion of HSP70 heat shock protein from cancer cells. The secretion of HSP70 helps to stimulate immune system cells against cancer and elicit a response from the cancer mass.
When it is used in combination with dendritic cancer vaccines, hyperthermia can further stimulate a cancer-specific T-cell response and increase the death of cancer cells.
In a case of breast cancer with liver metastasis that had rejected medical treatment, local hyperthermia with a dendritic cancer vaccine was successful for six years with good quality of life and no additional disease symptoms.
Primary tumor region hyperthermia with a 43°C temperature increase can increase the number of killer CD8+ T cells and activate dendritic cells, which help to stimulate the immune system against cancer. It is thought that regional hyperthermia may help to reduce disease recurrence or metastasis by stimulating the immune system.
Modern hyperthermia techniques can apply heat to cancer tumors in deep tissues without causing side effects using radiofrequency waves.
Reference:
1. Qin Y, Thorac Cancer 2016;7(4):422-7.
2. Hildebrandt B, Critical Reviews in Oncology/Hematology 2002; 43(1):33–56.
3. Tsang YW, BMC Cancer. 2015;15:708.
4. Schirmacher V, Immunotherapy. 2015;7(8):855-60.
5. Toraya-Brown S, Nanomedicine. 2014 ;10(6):1273-85.).
5. INTERLEUKIN-2(IL2) IMMUNOTHERAPY
Interleukin-2 (IL-2) is a cytokine used for over 35 years to stimulate the immune system. It promotes the proliferation of natural killer (NK) cells and anticancer T cells.
IL-2 is an immunotherapy drug that is used to treat various diseases, including cancer. It is effective in the treatment of renal cell carcinoma and melanoma. However, its use is limited due to the risk of side effects such as hypotension, capillary leak syndrome, albumin deficiency, electrolyte imbalance, and organ dysfunction when given intravenously.
A lower-dose subcutaneous form of IL-2 with fewer side effects is currently available. The combination of IL-2 with cancer vaccines generates a strong immune response.
The combination of stereotactic radiotherapy and high-dose IL-2 is an effective treatment of metastatic melanoma or renal cell cancer. IL-2 may be an alternative for patients who do not respond to treatment.
In phase 2 studies, the combination of low-dose IL-2 and colony-stimulating factors with chemotherapy has shown promise in the second-line treatment of chemotherapy-resistant small-cell lung cancer. The response rate in patients receiving chemotherapy and cytokine treatment was higher (58% versus 28%), and the median survival time was significantly longer (11.2 months versus 7 months) compared to patients who received chemotherapy alone.
These results are encouraging. IL-2 and zoledronic acid can be used together as an immunotherapy treatment for chemotherapy-resistant renal cell cancer, neuroblastoma, and other solid organ tumors. This treatment is administered through a subcutaneous injection and does not cause significant side effects. It works by increasing the number of γδ T cells, which help to recognize and kill cancer cells.
Radiation therapy is one of the options for the treatment of prostate cancer that has not metastasized. Studies are ongoing to increase the effectiveness of radiation therapy, particularly for patients who are hesitant to undergo surgical treatment due to its side effects. Studies have shown that the combination of metronomic low-dose IL-2 cytokine treatments with radiation therapy, along with cancer vaccination, is safe and provides a PSA response.
In metastatic malignant melanoma patients, applying IL-2 in combination with temozolomide chemotherapy showed a response in a subset of patients.
In metastatic renal cell cancer, applying low-dose vinorelbine in combination with IL-2 has been reported to result in long-term disease control.
In particular, clinical studies have shown that using IL-2 aerosol through the respiratory tract is safe for osteosarcoma cases with lung metastasis. Research is ongoing.
In summary, IL-2, which has been used as an immunotherapy drug for many years, is still one of the options available to us in cancer treatment today. There are scientific studies that suggest that it may be beneficial when used in combination with other immunotherapies or cancer treatments.
Reference:
1. Dhupkar P, Adv Exp Med Biol. 2017;995:33-51.
2. Pressey JG, Medicine (Baltimore). 2016; 95(39): e4909. Seung SK, Sci Transl Med. 2012;4(137):137ra74.
3. Lang JM, Cancer Immunol Immunother. 2011;60(10):1447-60.
4. Correale P, Cancer Biol Ther. 2009;8(6):497-502.
5. Lechleider RJ, Clin Cancer Res. 2008;14(16):5284-91.
6. Masucci GV, Melanoma Res. 2006 Aug;16(4):357-63.
7. Mencoboni MP, Neoplasma. 2006;53(4):333-6.).
6. High-dose Vitamin C
High doses of vitamin C applied intravenously have been proven to contribute to the supportive treatment of cancer in various clinical and preclinical studies, while there is no notable effectiveness of high doses of vitamin C applied orally.
Intravenous high doses of vitamin C reduce the inflammatory process in cancer patients. When vitamin C enters cancer cells, it is modified in a way that causes DNA damage and can enhance the effectiveness of chemotherapy or radiotherapy in killing cancer cells.
In clinical studies, long-term disease control with improved energy levels, appetite, and physical activity has been shown in some cancer patients who did not respond to standard treatment.
Reference:
1. Hoffer LJ, PLoS One.2015;10(4).
2. Mikirova N, J Transl Med 2012.
3. Sorice A, Mini Rev Med Chem. 2014;14(5):444-52.
4. O'Leary BR, Radiat Res. 2018 May;189(5):456-465.
7. Phytotherapy (Herbal medicine) and Dietary supplements
One of the areas where herbal and natural ingredients are most commonly used is in supporting the immune system. Many scientific papers and reviews have reported that they can provide benefits in this regard. Mushroom polysaccharides, astragalus memb, propolis, garlic, probiotics, ginseng polysaccharides, nigella sat, beta-glucan 1,3 1,6 branched, asparagus, cumin, chlorella strains, zinc, selenium, and caper orientalis are some of the natural/herbal products that are used to help support the immune system. One of the most common mistakes is using all of these supports together.
In our clinic, herbal treatments are used as complementary cancer therapy according to the type of cancer and the drugs used in the treatment.
Reference:
1. Huang CF, Cell Mol Immunol. 2008;5(1):23-31.
2. Ilyas U, Pharmacogn Rev 2016;10(19):66-70.
8. Alkalization therapy in cancer treatment
Cancer cells' metabolism leads to an increase in lactic acid production. The cancer cell pumps out the increased lactic acid within itself quickly by pumps to survive. As a result, an armor containing an acid layer forms outside the cancer cell. This armor reduces the entry of many cancer medicines into the cancer cell, reduces their effectiveness, and weakens the immune system.
In preclinical studies, using sodium bicarbonate orally and through the bloodstream, combined with cancer medicines, to reduce this acid has shown benefits in the treatment of certain cancers by inhibiting the pumps that excrete acid from cancer cells. In addition, reducing acidity in the cancer tumor with oral buffer solutions increases the effectiveness of immunotherapy drugs.
Alkaline cancer treatment is a complementary treatment, and is not used for every cancer treatment. Alkaline cancer treatments reduce the chances of recovery by impairing the effectiveness of drugs such as capecitabine and tyrosine kinase inhibitors.
Our clinic evaluates the suitability of alkaline cancer treatment based on the type of drugs used in cancer treatment and makes plans accordingly.
Reference:
1. Pilon-Thomas S, Cancer Res. 2016;76(6):1381-90.
2. Koltai T. Onco Targets Ther. 2016;9:6343-6360.
3. De Milito A, Future Oncol. 2005;1(6):779-86).
9. Anti-Inflammatory diet
Chronic inflammation in the body can cause the immune system to overwork and eventually become exhausted, which can also increase tissue damage. The presence of chronic inflammation in the body can increase the risk of developing cancer and accelerate the death of cancer patients.
It is essential to restrict the consumption of foods that promote inflammation and increase the consumption of anti-inflammatory foods to support the healing process. For example, after a breast cancer diagnosis, an anti-inflammatory diet consisting of whole grains, healthy fats, spices, and vegetables has been shown to help reduce the risk of death from heart disease in women. It is recommended to consume less saturated fat and more polyunsaturated fat, fruits and vegetables high in flavonoids, fiber, ginger, garlic, and green tea, which are good sources of antioxidants.
Adhering to healthy nutrition guidelines for cancer survivors can also help to reduce cancer recurrence risk.
At our clinic, we review the nutrition and lifestyle of cancer patients and create a personalized program with anti-inflammatory foods to help the healing process.
Reference:
1. Zheng Jiali, Research Conference on Food, Nutrition, Physical Activity and Cancer AICR 2011.
2. Mantovani A, Curr Mol Med. 2010;10(4):369-73.
3. Aune D. Transl Gastroenterol Hepatol. 2018;3:73.
10. Low-dose and metronomic chemotherapy
Cancer tumors contain Treg cells. These cells are a part of the immune system but inhibit the immune response. When the number of Treg cells increases, the immune response to cancer decreases, resulting in a shorter lifespan for cancer patients.
Specifically, some chemotherapy drugs applied at low doses in a metronomic manner reduce the number and function of Treg cells, thus increasing the response to cancer vaccines.
In addition to standard chemotherapy or immunotherapy, metronomic chemotherapy can stimulate an anti-cancer immune response. It may be beneficial when combined with other therapies to strengthen the immune system.
Reference:
1. Le DT, Cancer Res. 2012;72(14):3439-44.
2. Tongu M, Cancer Immunol Immunother. 2013;62(2):383-91
11. Physical exercises and Meditation
Regular exercise and stress-reducing activities such as meditation, prayer, and strengthening religious beliefs support the immune system. Cancer patients who regularly exercise can tolerate treatments better and have a higher chance of recovery. Therefore, it is recommended that cancer patients regularly engage in physical activity.
Reference:1. Fairey AS, Brain Behav Immun. 2005;19(5):381-8. 2. Betof AS, Brain Behav Immun. 2013;30 Suppl:S75-87).


